Platelet Rich Fibrin (PRF)
About Platelet-Rich Fibrin (PRF)
In oral and maxillofacial surgery, technology is continuously advancing, offering new ways to enhance patient care and outcomes. One of the most exciting developments in this field is the use of Platelet-Rich Fibrin (PRF). Since its introduction in 2001, PRF has been utilized to accelerate healing following surgical procedures, making recovery faster and more comfortable for patients.
What Is PRF?
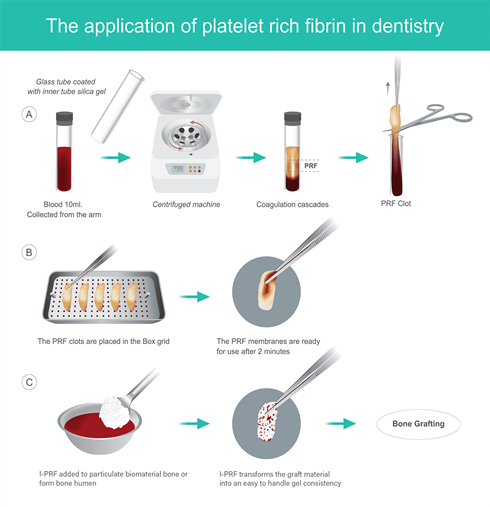
Platelet-Rich Fibrin (PRF) is a concentrated form of your own blood components, specifically designed to enhance the body’s natural healing processes. When you choose to incorporate PRF into your oral surgery, a simple blood draw is performed, similar to a routine medical test. The blood is then processed in a centrifuge, which separates and condenses the fibrin, platelets, and white blood cells into a structured, resistant mesh. This PRF mesh is rich in growth factors that significantly enhance healing, making it an ideal addition to your surgical procedure.
Composition of PRF
Leukocytes (White Blood Cells): These cells are essential for your body’s defense against infection. In PRF, leukocytes provide antibacterial properties, helping to ward off infections and promote healthy healing.
Platelets: Platelets play a crucial role in wound healing by initiating the clotting process and releasing growth factors. In PRF, platelets are embedded within the fibrin mesh, delivering growth factors directly to the surgical site, which accelerates healing.
Fibrin: Fibrin is an insoluble protein that forms the foundation of blood clots. In PRF, fibrin creates a scaffold that supports cell movement and tissue regeneration at the surgical site.
- Stem Cells: These undifferentiated cells have the unique ability to become different types of cells needed for tissue repair and regeneration. The presence of stem cells in PRF contributes to its powerful healing capabilities, often referred to as “stem cell dentistry.”

PRF in Oral Surgery Procedures
PRF is a versatile tool in oral surgery, offering enhanced healing in various procedures:
Extractions: PRF helps promote faster healing and significantly reduces the risk of developing a dry socket after tooth extraction.
Dental Implants: PRF accelerates the healing process and supports the osseointegration of implants, potentially reducing recovery time from three to six months.
Bone Grafting: When combined with bone graft material, PRF stimulates bone growth and speeds up the healing process, ensuring better outcomes for patients.
Benefits of Platelet-Rich Fibrin
The recovery process is often a concern for patients undergoing oral surgery. PRF offers several benefits that make the healing process faster and more comfortable:
Enhanced Healing: PRF facilitates faster tissue regeneration, reducing pain, swelling, and recovery time.
Reduced Risk of Infection: PRF’s antibacterial properties help protect the surgical site from infection.
Improved Bone Formation: PRF attracts bone-forming cells, assisting in the integration of bone grafts and the formation of new bone.
Prevention of Dry Socket: PRF helps hold blood clots in place after extractions, significantly lowering the risk of dry socket.
Safe and Natural: Since PRF is derived from your own blood without any chemical additives, it is a safe and effective natural healing agent.


The Science Behind PRF
PRF is a concentration of platelets, leukocytes, and fibrin obtained from your own blood through centrifugation. The platelets in PRF release growth factors such as PDGF and TGF-β, which accelerate healing by stimulating tissue regeneration, new blood vessel formation, and collagen production. Leukocytes contribute to an immune response, preventing infection, while the fibrin matrix provides a supportive scaffold for cell movement and repair at the surgical site.
Preparing for a PRF Procedure
Before undergoing a procedure with PRF, you should:
- Inform your healthcare provider about your medical history, including any medications or allergies.
- Avoid medications or supplements that could affect blood clotting, as advised by your surgeon.
- Stay hydrated and eat a normal meal before the procedure to maintain stable blood sugar levels.
Timeline for PRF Benefits
The benefits of PRF vary depending on the procedure and individual health but generally follow this timeline:
- Initial Healing: Reduction in inflammation and pain within the first few days.
- Mid-term Healing: Tissue regeneration and new blood vessel formation occur over the following weeks, critical for soft tissue and bone healing.
- Long-term Healing: The full benefits, especially for bone grafting or dental implants, emerge over several months as PRF supports stable and robust healing.
Contact Us
For more information or to schedule an appointment, please contact us. Dr. Dieu and the team at PREMIER ORAL & FACIAL SURGERY are here to guide you through your treatment options and help you achieve the best possible outcomes.
Frequently Ask Questions
Is PRF safe?
Yes. PRF is derived from your own blood, making it a safe and natural option. The process is quick, with PRF being ready to use in less than 15 minutes.
Should PRF be used in all bone-grafting cases?
Not always, but in most cases, PRF enhances the outcome by increasing bone volume and speeding up the healing process.
Will my insurance cover the costs?
Unfortunately, PRF is typically not covered by insurance. However, the cost to the patient is minimal.
Can PRF be used alone to stimulate bone formation?
No. PRF must be combined with bone graft material, such as the patient’s own bone, a bone substitute, or a synthetic product like BIO-OSS.
Are there any contraindications to PRF?
Patients with bleeding disorders or hematologic diseases may not be eligible for PRF. Consult with your surgeon and primary care physician to determine if PRF is right for you.
Do I need PRF for a tooth extraction?
PRF is highly beneficial for tooth extractions, as it protects the site from infection and accelerates the healing process.
Can you still get a dry socket with PRF?
PRF significantly reduces the risk of dry socket, lowering the likelihood from 1 in 10 to about 1 in 100.

